TEl: +86-13148388090
Fax:+86-571-88616515
How Does a Suction Catheter Work
Author: admin / 2024-09-10As we know, suction catheters are used to remove secretions such as mucus, saliva, blood, or other fluids from a patient's airway, trachea, or lungs. Understanding how it works will improve our grasp of this kind of product, which in turn helps a lot if you are concerned for a person with problems that need to be solved with a suction catheter.
What Is a Suction Catheter
A suction catheter is a medical device used to remove secretions such as mucus, saliva, blood, or other fluids from a patient's airway, trachea, or lungs to help them breathe more easily. It is typically a long, flexible tube inserted into the airway via the mouth, nose, or through a tracheostomy tube.
Different Types of Suction Catheters
Suction catheters are available in various types, each designed for specific purposes and patient needs. Different types of suction catheters are described below.
1) Flexible Suction Catheter
Description: A soft, flexible tube that can be inserted deeper into the trachea or bronchial tree.
Usage: Often used for patients with endotracheal or tracheostomy tubes. It is inserted into the trachea to remove secretions from the lower airways.
Advantages: The flexibility allows it to navigate the airway more easily and reach deeper into the lungs.
2) Coude Tip Suction Catheter
Description: A flexible suction catheter with a slightly angled or curved tip.
Usage: Designed to access specific areas of the airway, particularly the left mainstem bronchus, which can be difficult to reach with a standard straight catheter.
Advantages: The angled tip allows for more targeted suctioning, especially in difficult-to-reach areas.
3) Whistle Tip Suction Catheter
Description: A catheter with a side hole near the tip, reducing the risk of trauma during suctioning.
Usage: Used in patients with delicate airway tissues or when a gentler suction is needed.
Advantages: The design minimizes the chance of mucosal damage, making it safer for patients with sensitive airways.


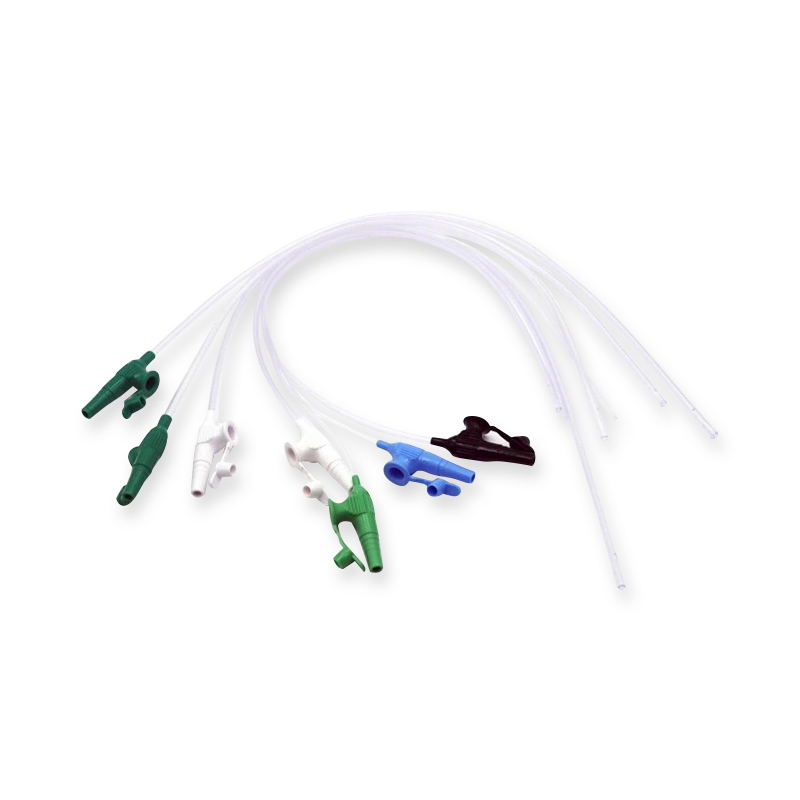
If you want to see how an actual catheter of this type looks like, refer to the picture below from Hangzhou Bever Medical Device Co., Ltd.
4) Argyle Suction Catheter
Description: A flexible catheter with multiple eyes (holes) at the tip.
Usage: Typically used for suctioning secretions from the trachea and bronchial tree.
Advantages: The multiple eyes help ensure consistent suctioning and reduce the risk of tissue adherence and trauma.
5) Silicone Suction Catheter
Description: Made from soft silicone, this catheter is more pliable and less likely to cause trauma to the airway tissues.
Usage: Used for patients with sensitive airways or when repeated suctioning is necessary.
Advantages: The soft material is gentle on the tissues, reducing the risk of irritation or damage.
How Does a Suction Catheter Work
A suction catheter works by removing fluids, secretions, or debris from a patient's airway to help maintain clear breathing. A suction catheter helps keep the airway clear of obstructions that can impede breathing, providing essential respiratory support for patients in various medical settings, from emergency care to post-surgical recovery and intensive care.
The steps below shows how it works.
1) Connection to Suction Machine
The suction catheter is connected to a suction machine or a wall-mounted suction unit. This machine generates negative pressure, creating a vacuum that helps draw out fluids from the body.
2) Insertion into the Airway
The suction catheter, typically made of flexible material, is gently inserted into the patient’s airway, either through the mouth, nose, or a tracheostomy tube (if applicable). For deeper suctioning, it can be introduced into the trachea or bronchial passages.
Care must be taken to avoid trauma to the airway during insertion.
3) Application of Suction
Once the catheter reaches the desired location, suction is applied by covering a small control valve or hole (often called a "thumb port") on the catheter or suction line. This action creates a vacuum at the catheter’s tip, allowing it to pull out secretions.
The catheter is gently rotated or withdrawn slowly to collect secretions without causing airway injury.
4) Collection of Secretions
As the catheter suctions fluids, they are transported through the catheter tubing and into a collection chamber attached to the suction machine. This chamber holds the removed mucus, blood, saliva, or other fluids for disposal.
5) Removal and Cleaning
After the suctioning procedure, the catheter is removed carefully from the airway. In cases where the catheter is disposable, it is discarded after use. Reusable catheters, however, must be cleaned and sterilized before the next use.
The airway is evaluated to ensure it is clear, and additional suctioning may be performed if needed.
6) Maintaining Oxygenation
If the patient is on oxygen or a ventilator, suctioning may briefly interrupt the flow of oxygen. For this reason, closed suction systems or techniques like hyperoxygenation before suctioning are used to minimize oxygen loss, especially in critically ill patients.
How to Use a Suction Catheter
Preparation
Gather Supplies
Suction catheter (correct size for the patient)
Suction machine or wall-mounted suction unit
Sterile gloves
Sterile water or saline (for lubricating and cleaning the catheter)
Suction tubing
Collection canister (connected to the suction unit)
Personal protective equipment (PPE), including mask and goggles (if required)
Set Up the Suction Machine
Connect the suction catheter tubing to the suction machine or wall unit.
Ensure the suction unit is working and set the pressure to a safe range:
Adults: 100–150 mmHg
Children: 100–120 mmHg
Infants: 80–100 mmHg
Preterm neonates: 60–80 mmHg
Ensure Sterility
Wash your hands and put on sterile gloves.
If using an open suction system, maintain sterility of the suction catheter by handling only the proximal end (the part that connects to the tubing).
Position the Patient
Position the patient in a semi-Fowler's or upright position to help facilitate easier access to the airway and to optimize lung expansion.
If the patient is unconscious or cannot sit upright, lateral positioning or head tilt may be used.
Pre-Oxygenation (if necessary)
For patients on oxygen or a ventilator, consider giving them supplemental oxygen for 30–60 seconds before suctioning to prevent oxygen desaturation.
Suctioning Process
Insert the Suction Catheter
Gently insert the suction catheter into the patient's airway (nose, mouth, or tracheostomy) without applying suction yet.
If suctioning the trachea, advance the catheter carefully until you feel resistance (about 10-15 cm for adults), then withdraw slightly before applying suction.
Apply Suction
Apply suction by covering the control port or valve on the catheter while slowly withdrawing the catheter.
Rotate the catheter between your fingers as you pull it out to ensure all areas of the airway are reached.
Limit suctioning to 10-15 seconds per pass to reduce the risk of hypoxia (oxygen deprivation).
Clear the Catheter
After each suction pass, clear the catheter by dipping it into sterile water or saline and applying suction to rinse out any mucus or secretions trapped inside.
If necessary, repeat the process of suctioning and clearing until the airway is clear of secretions.
Monitor the Patient
Throughout the process, observe the patient for signs of distress, oxygen desaturation, or changes in vital signs.
Stop suctioning immediately if the patient shows any signs of discomfort, respiratory distress, or bradycardia (slow heart rate).
Post-Suctioning Care
Reassess the Patient
Check the patient’s respiratory status, including oxygen saturation levels, breath sounds, and overall comfort.
Administer supplemental oxygen if required to help the patient recover from the suctioning procedure.
Clean and Dispose of Equipment
If the catheter is single-use, discard it immediately in a biohazard waste container.
If using a reusable suction catheter, clean it with sterile water and follow sterilization procedures according to your facility’s protocols.
Document the Procedure
Document the procedure, including the number of suction passes, the patient’s response, the type and amount of secretions removed, and any complications.
Conclusion
We hope this article explains clearly how a suction catheter works. By knowing how it works, people interested in suction catheters will be more informed on how to make it provide optimal medical benefits. If you want to delve into this product, you can visit a website such as this one: www.bevermedical.com.


